Using the body’s natural mechanisms to reverse the course of diseases of the eye
Ocugenix is developing therapies for angio-fibrotic diseases of the eye such as wet macular degeneration and diabetic retinopathy. These diseases are caused by an aberrant wound response in the back of the eye. Ocugenix’s compound triggers the process of wound resolution to cause the regression of the excessive fibrosis and vasculature recruited to heal the wound. The ability to cause regression of the pathological vessels and fibrosis in AMD and DR offers the patient the best hope of restoring lost sight.
Welcome to
OCUGENIX
Ocugenix was founded by a nationally recognized research team from the University of Pittsburgh Medical Center and based on over 20 years of NIH-funded research into the molecular mechanisms of wound healing and cellular response. The company has assembled an experienced development team with expertise in clinical design, science, regulatory, toxicity, and CMC. Combined, the team has taken over 50 products through the ophthalmology section of the FDA to market.
Ocugenix is focused on the development and commercialization of therapeutics for ocular diseases caused by excessive fibrosis and blood vessels in the eye.
The Company’s lead asset is Ocu-110, a small molecule drug candidate designed to limit both the fibrosis and angiogenesis that are characteristic of these diseases. The company expects to begin its first-in-human clinical trials of the compound in 2023.
Angiopathies of the Eye
Macular Degeneration and Diabetic Retinopathy
Wet age-related macular degeneration (AMD) and proliferative diabetic retinopathy are leading causes of blindness with more than 3 million people being treated annually in the US alone. Similar prevalence are noted in all OECD countries, with lower but climbing prevalences in emerging economies.
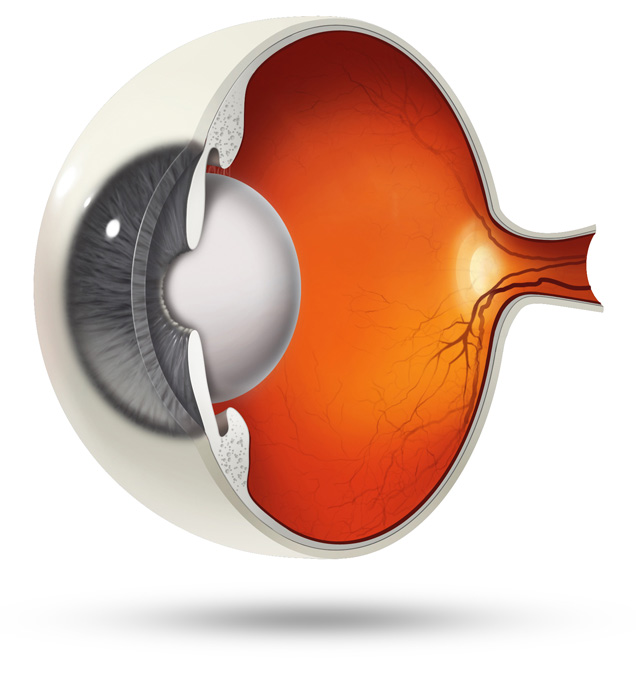
In wet AMD, an aberrant wound response leads to the proliferation of blood vessels along with a fibrotic reaction into the macula, the area of the retina responsible for processing central vision. Damage to photoreceptors in the macula can cause distortion or blind spots in a person’s central vision. Patients with wet AMD who are untreated or for whom treatment is ineffective can progress to total blindness. VEGF inhibitors address the edema released by this pathological vasculature but do nothing to cause the regression of the vessels or limit the fibrosis that are responsible for the long-term loss of sight. This is an unmet clinical need that is not addressed by the other compounds in development for AMD.
In diabetic retinopathy, abnormal, “leaky” blood vessels infiltrate the retina and the vitreous cavity, which leads to the formation of fibrotic tissue on the retinal surface or in the vitreous cavity, vitreous hemorrhage, retinal detachment, retinal damage, and loss of vision. Laser photocoagulation is often effective, but the procedure can be painful and result in loss of peripheral vision. Anti-VEGF therapies are effective for a large percentage of patients, but as many as 25% do not respond and many more become resistant over time.
Science
Ocu-110 is a small molecule drug candidate that selectively activates the CXCR3 pathway, which is the pathway most strongly implicated in pruning neovascularization and limiting fibrosis in wound healing. While existing treatments block a single growth factor that drives vascular proliferation (such as VEGF), Ocu-110 targets a pathway that over-rides all the numerous factors that drive angiogenesis and fibrosis. By activating CXCR3, Ocu-110 causes regression of both the abnormal blood vessels and fibrotic tissue, leaving the pre-existing vascular and fibrotic infrastructure in place.
Mechanism of Action
Ocu-110 selectively activates the CXCR3 pathway via the physiologic binding site. The CXCR3 pathway has been well characterized in wound healing, where it regulates fibrosis and angiogenesis. This pathway restores wound healing toward a regenerative state by noncompetitively over-riding pro-angiogenic and pro-fibrotic signals from a variety of growth factors including VEGF.
In retinal diseases, activating this same pathway is expected to produce an anti-fibrotic and angio-regressive effect that would not only arrest disease progression but potentially reverse it. Ocu-110 is derived from a naturally occurring activator of the CXCR3 pathway that has been vetted in preclinical studies, in which it was shown to regress vascularization and inhibit fibrosis. As it is a physiologic activator of CXCR3, there has been no evidence of toxicity in any of our preclinical studies.